
Parkinson’s Disease is Singapore's second most common neurodegenerative disorder and affects about 0.3% of Singapore residents aged 50 years and above
Holding a pen, feeding yourself, or even putting clothes on – when was the last time you paid attention to these simple habitual actions? For people with Parkinson’s, doing these things can become a challenge as the condition can affect daily activities.
Check out our guide for caregivers of seniors with Parkinson’s Disease, or if you are seeking to first understand this condition, read on.
What is Parkinson’s and what causes it?
Parkinson’s disease (PD), or simply Parkinson’s, is a long-term degenerative disorder in the central nervous system where nerve cells are impaired or no longer function. This mainly affects motor functions, but is known to also affect memory, speech, swallowing, mood and behaviour.
While the cause of the condition is not fully understood, the onset of Parkinson’s Disease is attributed to the lack of dopamine, a chemical that helps to relay messages in our brain and regulate happy moods. It is a progressive condition, beginning with gradual symptoms in early stages, to a debilitating condition in later stages.
Based on a study in 2004, about 0.3% of Singapore residents aged 50 years and above have Parkinson’s Disease. With an ageing population, the numbers will likely increase further.
What are the different stages of Parkinson’s?

Parkinson’s Disease affects about 0.3% of Singapore residents aged 50 years and above
There are broadly 5 stages for Parkinson’s Disease. Each stage impacts each patient and their caregiver differently. A diagnosis from a medical professional can inform which of the five stages your loved one is experiencing:
Stage One
During the initial stage, the patient experiences mild symptoms like clumsiness, stiffness in posture and slowed facial expressions. These generally do not interfere with daily activities. Tremors and slowness of movement tend to occur on one side of the body only.
Stage Two
Tremors, rigidity and other movement symptoms begin to get worse, affecting both sides of the body. The patient is still able to live independently, but daily tasks such as walking, bathing and changing clothes become more difficult to complete and take a longer time. Other symptoms include decreased blinking, speech abnormalities, and stiffness in trunk muscles.
Stage Three
The mid-stage of Parkinson’s is characterised by loss of balance and slowed movements, also known as bradykinesia. The patient is still mostly independent, however the symptoms of Parkinson’s significantly hinder daily activities such as feeding or changing themselves. Caregivers should watch out for falls, as these become more common.
Stage Four
The symptoms of Parkinson’s limit the movement of the patient. He or she requires assistive devices such as canes or walkers, to move about without falling. While he or she can still stand, the patient will need help with activities of daily living such as bathing and moving about, and may require a caregiver.
Stage Five
At the last stage of Parkinson’s, stiffness in the legs makes walking or standing difficult or impossible. The patient is bedridden, or requires a wheelchair to move about with the help of a caregiver. Round-the-clock nursing care is required for all daily activities, and swallowing food becomes difficult.

Patients are more likely to seek a doctor’s diagnosis at stages two and three when they notice motor symptoms that affect their lifestyle
Symptoms of Parkinson’s and When To See A Doctor
The diagnosis for Parkinson’s usually occurs between stages two and three, as patients are more likely to seek a doctor’s diagnosis when they notice that the motor symptoms are beginning to affect their lifestyle. While not all Parkinson’s patients have the same set of symptoms, it is helpful to keep an eye out for general motor symptoms of Parkinson’s by remembering the abbreviation, T.R.A.P. (Tremors, Rigidity, Absence or Slowness of Movement, Postural Instability):
Tremors
Tremors affect 70-80% of Parkinson’s patients. One of the more common tremors is the pill rolling tremor, which looks like a person rolling a pill or a small object between their thumb and index finger, and happens when the hand is at rest. Tremors can also occur in the hands, on the lower jaw and legs.
Rigidity
Involuntary stiffness of bodily muscles and a sensation of tightness are some of the symptoms of Parkinson’s. This results in decreased flexibility, limited facial expressions, and sometimes a hunched back. Rigidity can also make it difficult for a patient to perform daily tasks well.
Absence or Slowness of movement
Also known as bradykinesia, this is often described as the feeling of having feet “glued to the floor” or “freezing”. It can appear as a shuffling gait, or a person taking smaller steps. Freezing can also happen in the hands or when speaking.
Postural instability
Keeping balanced when standing still, getting up from a chair, or walking becomes difficult and can lead to an increase in falls, twice as often as someone of the same age who is healthy.
On top of these motor symptoms, some other symptoms may include digestive issues, difficulties with swallowing, depression, fatigue, sleep problems, pain, and forgetfulness.
If your loved one is experiencing a combination of these symptoms, bring them to see a neurologist.
How is Parkinson’s diagnosed?
A movement disorder specialist, who is a specialised neurologist may diagnose Parkinson’s based on your loved one’s medical history, neurological and physical examinations. For example, the doctor may ask for family history and observe the patient’s movements.
Medications that help increase dopamine in the brain are the first line of treatment for Parkinson’s patients
How is Parkinson’s treated?
We know that there is no cure for Parkinson’s, so managing the condition with medication is the first line of treatment for symptoms and slowing the progression of the disease. Some of these medications that help control tremors, rigidity and slowness of movement include dopamine agonists to mimic dopamine in the brain and others that synthesise or retain the effect of dopamine.
Movement disorder specialists rely on their clinical examination and patient’s feedback towards the treatment to create a tailor-made medication regime. This is why keeping up with doctor appointments is so important!
Families may also consider getting help from care and therapy services to help in their quality of life and reduce caregiving stress.
Risk factors for Parkinson’s
There are currently no existing tests to tell for sure if our loved ones will develop Parkinson’s in the future. However, many studies have been carried out to identify the risk factors for Parkinson’s.
Your risk of developing Parkinson’s increases if you are:
- Male and above 60 years old. Men have twice the risk of developing Parkinson’s than females, though this trend on gender and age is less noticeable in Asia.
- Exposed to pesticides and heavy chemicals. Research shows that exposure to chemicals like pesticides, herbicides, heavy metals and solvents are linked to a relatively small risk in developing Parkinson’s.
- Genetically predisposed to developing Parkinson’s. About 10 to 20 percent of Parkinson’s disease cases are linked to a genetic cause.
Summary
Parkinson’s Disease is a complex condition that affects everyone differently. As family members, we can be better prepared for the caregiving journey by understanding the signs and symptoms, and learn how to best support our loved ones who are going through this condition. For helpful tips, read our guide for caregivers of seniors with Parkinson’s.
Frequently Asked Questions
- What is Deep Brain Stimulation and is it a cure for Parkinson’s?
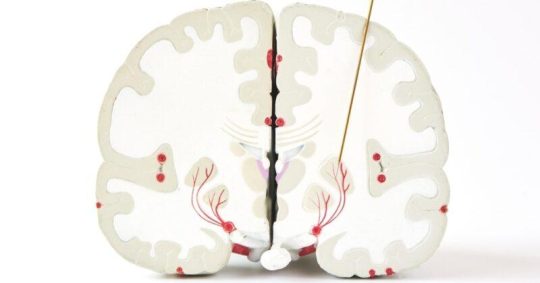
Deep Brain Stimulation is a procedure where the patient has two electrodes placed in specific areas of their brain. They are connected to a battery below the patient’s collar bone and light currents of electricity are used to regulate abnormal brain impulses or control certain chemicals in the brain. These are done with the aim of relieving Parkinson’s symptoms like tremors, rigidity and slowed movement.
Deep Brain Stimulation is not a cure for Parkinson’s Disease, but research has shown it to reduce the severity of symptoms and amount of medication needed, even 5 years after the surgery¹.
Due to the surgical risks, this procedure is recommended for patients aged 70 and below, and may be used as a last resort for patients who cannot tolerate the medications or have severe motor fluctuations.¹Deep brain stimulation in early-stage Parkinson disease (Source)
- How quickly does a patient deteriorate from each stage of Parkinson’s?
Every Parkinson’s case is different and progresses at different rates. In general, it may take 20 months for someone to move across from stage 1 to 2; from stage 2 to 3, about 85 months, from stage 3 to 4, about 24 months and from stage 4 to 5, about 26 months.
- How long do people live with Parkinson’s?
People diagnosed with Parkinson’s can lead a normal lifespan if they manage their health appropriately. Continue to follow a healthy diet and stay active to slow down the effects of immobility. Consult your doctors and allied health professionals to develop a management plan.
- Will I ever recover from Parkinson’s?
There is ongoing and extensive research on finding a cure for Parkinson’s. It is important to take on a positive outlook to prepare for the medical breakthrough that could happen one day.
Get in touch with us
If you are looking for professional services in Singapore to help to support your loved one with Parkinson’s, visit our Parkinson's Care page.
NTUC Health offer Parkinson's Exercise Classes as well as rehabilitation and therapy. Other resources can be found in the Parkinson's section of our blog.


