If you find your knees hurting when you walk or try to climb the stairs, or the stiffness in your joints causes you to feel discomfort, you may have osteoarthritis in the knee. Just like a trusty hinge that allows a door to swing open and closed smoothly, our knee joint is a remarkable mechanism that enables us to move with ease. However, wear and tear of the cartilage can accumulate over time, and the persistent pain in your knee is a signal that your body is sending you to seek treatment.
A diagnosis of osteoarthritis knee is made clinically where the doctor will conduct a physical examination and look through your medical history. This would include checking the affected knee for tenderness, swelling, flexibility and range of motion. Additional laboratory tests and X-rays may be needed to look for narrowing of the joint space, bone and cartilage damage or the formation of bone spurs.
In this article, we will cover the following topics:

Photo credit: Samitivej Hospital
What is osteoarthritis
As we grow older, the gradual wear and tear on our joints can result in cartilage deterioration, leading to the experience of chronic pain, stiffness, and diminished mobility. Osteoarthritis, often referred to as "wear and tear" arthritis, is a degenerative joint disorder that most commonly affects the knee joint. According to WHO (World Health Organization) data1, about 60% of people living with osteoarthritis are women, and about 73% are older than 55 years old.

What causes knee osteoarthritis
Typically, the incidence and prevalence of osteoarthritis increases with age, with many in their late 40s to mid-50s experiencing symptoms. It can also affect younger individuals, in particular athletes and someone who had previously sustained joint injury or trauma. It is important to know that osteoarthritis of the knee is not simply a direct consequence of ageing. Singapore’s Ministry of Health (MOH) estimates that about 40% of those above 70 years old suffer from knee osteoarthritis.
Risk factors that can cause knee osteoarthritis:
- Age: Knee osteoarthritis has been found to increase with age, especially after 40 years old2. As we grow older, the cartilage in the knee joint starts to gradually wear away and the underlying bone and tissue begins to change with reduced ability to repair itself. The water content in the cartilage decreases and makes the knee less mobile, so the surrounding muscles weaken and become less supportive.
- Genetics: Genetic predisposition plays a significant role in whether an individual will develop knee osteoarthritis. If your parents or close relatives have had knee osteoarthritis, you are at a higher risk of having it too.
- Obesity: Excess body weight places added stress on the knee joints, accelerating the breakdown of cartilage. This is particularly significant for the knee joints, which support much of our body weight during activities.
- Joint injuries: Previous injuries or trauma to the knee, such as ligament tears or fractures, can increase the risk of developing knee osteoarthritis later in life.
- Pre-existing diseases: Joint diseases such as rheumatoid arthritis or gout, or even diabetes places a person at risk of developing knee osteoarthritis. Those with certain metabolic disorders, such as iron overload or excess growth hormone, are also at higher risk of knee osteoarthritis.
- Occupational and lifestyle factors: Jobs that involve repetitive stress on the knees or require constant kneeling can contribute to the development of knee osteoarthritis. Similarly, a sedentary lifestyle can weaken the muscles around the knee, leading to joint instability.
Symptoms of knee osteoarthritis
Knee osteoarthritis begins with pain usually, and this can be worsened by weight bearing and relieved by rest, but will likely become persistent as the condition becomes more severe. Symptoms are usually progressive when you have osteoarthritis of the knee. Changes may happen gradually over time but depending on the severity of your condition, you may even find it difficult to extend and bend your leg.
Recognising the symptoms of knee osteoarthritis is important for early diagnosis and management:
- Pain and stiffness: The earliest symptom is a sharp discomfort or a deep ache, often aggravated by activities like walking, climbing stairs, or even sitting for extended periods of time. Individuals with knee osteoarthritis tend to also experience joint stiffness, especially in the morning or after periods of inactivity.
- Weak muscles: As the joint becomes less stable and impacting overall leg strength and balance, muscles surrounding the knee may weaken.
- Swelling: The knee joint may become swollen due to inflammation caused by the breakdown of cartilage.
- Limited range of motion: Osteoarthritis can lead to a decreased ability to fully bend or straighten the knee.
- Crepitus: You might notice a grinding or crackling sensation that can occur when moving the knee, caused by the roughened bone surfaces rubbing against each other. Crepitus can also occur with movement pain.
Early diagnosis and appropriate treatment can help slow down progression and improve the quality of life for individuals living with knee osteoarthritis.
Previous knee injuries may lead to joint wear and tear and bone spurs (osteophytes). However, it is important to note that bone spurs cause no symptoms on the early onset and can go undetected for years, but can become especially painful when they start to press on nerves or tendons.
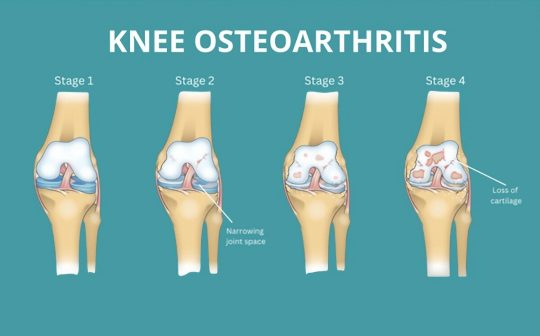
Knee graphics from Spring loaded technology
The four stages of knee osteoarthritis
Knee osteoarthritis is typically categorised into four stages, each representing the extent of the condition:
Stage 1 - Early or Minor Osteoarthritis
There might be minor wear and tear in the cartilage, but the joint space remains relatively normal. Individuals might experience mild discomfort or occasional pain after physical activity. X-rays might not show significant changes yet.
Stage 2 - Mild Osteoarthritis
The cartilage continues to deteriorate and joint space might begin to narrow. Individuals might experience more frequent pain, stiffness, and reduced flexibility, particularly after physical exertion. X-rays could start showing noticeable changes in the joint structure.
Stage 3 - Moderate Osteoarthritis
Pain, stiffness, and limited joint movement become more prominent as the cartilage starts to erode, impacting daily activities. Individuals might find it challenging to bend, squat, or climb stairs. Bone spurs could develop around the joint and at this stage, X-rays often reveal significant changes in joint structure.
Stage 4 - Severe Osteoarthritis
As joint deformity becomes noticeable and bone spurs grow larger, it is likely that there will be persistent knee pain and limited mobility, even during rest. Daily activities become extremely difficult. X-rays will likely show marked deterioration of the joint structure.

Types of treatment available
A healthcare professional, such as a general practitioner or physiotherapist, can provide accurate assessments and treatment recommendations based on an individual's specific situation.
While knee osteoarthritis is a chronic condition and the damage to the joints cannot be reversed, various treatment strategies can prevent further deterioration, reduce pain, improve mobility, and enhance overall quality of life:
- Lifestyle modifications: Maintaining a healthy weight or losing weight through proper diet and exercise can significantly reduce stress on the knee joints. Studies show that those who exercise regularly typically experience less pain.
- Physiotherapy: Targeted exercises can strengthen the muscles around the knee, providing better support and stability and helps improve range of motion.
- Medications: Over-the-counter pain medications, or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed by the doctor can help manage joint pain and inflammation.
- Home-based assistive devices: Using devices like a knee brace, a compression sleeve or a walking cane can provide added support and reduce strain on the knee joint.
- Injections: For short-term improvement of symptoms, your healthcare provider may prescribe corticosteroid injections, but regular use of intra-articular steroids is not recommended.
- Surgery: While the initial treatment is nonsurgical, in severe cases, surgical interventions like knee arthroscopy (to remove damaged cartilage and bone) or knee replacement surgery may be considered to restore joint function and reduce pain
How much will it cost for treatments
Fees vary based on the treatment mode of service required. For physiotherapy options, please refer to the following pages:
Does insurance cover the cost of treatment?
For surgery claims, out-of-pocket expenses, exclusions and direct billing arrangements, you will need to check with your private health insurance provider. Many health insurance plans cover physiotherapy in Singapore, but you may need a doctor’s referral letter for physiotherapy to make an insurance claim for your treatment.
To get a doctor’s referral letter, make an appointment to visit our Family Medicine Clinic.
If you would like to find out if you are eligible for any financial assistance, visit our subsidies page here.
Exercises suitable for knee osteoarthritis
Physiotherapy and regular exercise can be a game-changer in managing knee osteoarthritis and offers a holistic path to pain relief. Starting with stretch or strengthening exercises and low-impact activities like tai chi and water aerobics are also beneficial for improving flexibility, strength, and muscle control for osteoarthritic knees. However, always consult a healthcare professional before starting any new exercise routine.
Stretching Exercises

Hamstring stretch: Sit on the chair with legs extended and lean forward for a back-of-thigh stretch. For a standing version, stand upright and with one hand use a chair for support, place one leg onto a stool. Keep the leg straight and lean forward.

Calf stretch: Face a wall and place both your palms on it. Step one leg back, keeping toes forward. Bend your front knee while keeping your back leg straight and both heels on the ground. Stretch your calf and hold for 20-30 seconds. Ensure you don’t point your toes sideways.

Quadricep stretch: Stand upright and with one hand use a chair for support. Grab your ankle with the other hand, pull heel to buttock for a front-thigh stretch. Hold for 20-30 seconds, keeping your knees close together. You could also modify this stretch by lying on your side and stretching with a towel.
Strengthening Exercises
Hold for 10 seconds, repeat 10 times, and do 2 to 4 sets each.

Straight leg raise: Lie on your back with one knee bent. Raise the other leg 6-10 inches, hold for 10 seconds, then lower gently.

Hip abduction: Lie on your side with the bottom leg bent. Lift your upper leg horizontally and keep it straight, hold for 10 seconds, then lower it down.

Hip extension: Lie flat on your stomach and raise one leg while keeping both knees straight. Hold for 10 secs then lower it down.

Wall squats: Standing with your back against a wall, take 1 to 2 steps forward and gradually lower your body, hold for 10 seconds. Ensure you keep your knees shoulder-width apart, toes forward. To ensure that the exercise is effective, don’t bend your knees over your toes.

Seated knee extension: Sit on the edge of a chair, straighten one knee, hold 10 seconds, lower your foot back down.

Heel raises: Stand upright and place both hands on a chair. Raise your heels, hold 10 secs then relax and lower them.

Taking the First Step: Seeking Expert Care
Remember, osteoarthritis is a prevalent joint condition which affects weight-bearing joints like hips and knees that can disrupt daily life, which is why early intervention is crucial to avoid worsening the knee’s condition. Seek help from experienced physiotherapists who have a deep understanding of how to manage osteoarthritis.
Summary
To help you get started on a personalised treatment plan focused on pain relief, improving joint function, and enhancing mobility, NTUC Health has an experienced physiotherapy and rehabilitation team and comprehensive range of elderly-friendly equipment.
Explore our Rehabilitation and Physiotherapy Centres located islandwide.
After your first consultation, you can also opt for tele-rehabilitation service so you can save on travelling time and rehabilitation with our therapists over a video call. For caregivers with a family member who is unable to travel out of their home, home therapy where a physiotherapist makes a home visit to carry out the session might be an option for you.
References
1. GBD 2019: Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. https://vizhub.healthdata.org/gbd-results/
2. Leung YY, et al (2018) Validation of screening questionnaires for evaluation of knee osteoarthritis prevalence in the general population of Singapore. International Journal of Rheumatic Diseases, 21: 629-638.


